Trabecular Meshwork Regeneration in Primary Open Angle Glaucoma
Trabecular Meshwork cell stress impedes the function of the tissue
Elevated intraocular pressure (IOP) is a strong risk factor for the development of glaucoma. The trabecular meshwork (TM) is vital in the regulation of IOP. Our studies have shown that expression of damaged or mutated proteins in trabecular meshwork cells can lead to cellular stress that eventually results in the death of the cell. TM cell loss, in turn, leads to dysfunction of the tissue and increased IOP. TM cell stress can also be brought about by environmental factors or simply by advanced age.
Can the glaucomatous trabecular meshwork be repaired?
Lowering IOP using eye drops has reduced the amount of vision loss in a very large number of glaucoma patients, but requires daily application of drops for the rest of the patient's life. Unfortunately, patient compliance is poor, leading to insufficient control of the IOP. We believe that replacement of damaged or lost trabecular meshwork (TM) cells with healthy cells can lead to functional restoration following transplantation into glaucoma eyes. TM cell replacement could preserve or restore aqueous humor outflow facility and decrease IOP. This approach would free patients from daily eye drop regimens and avoid non-compliance .
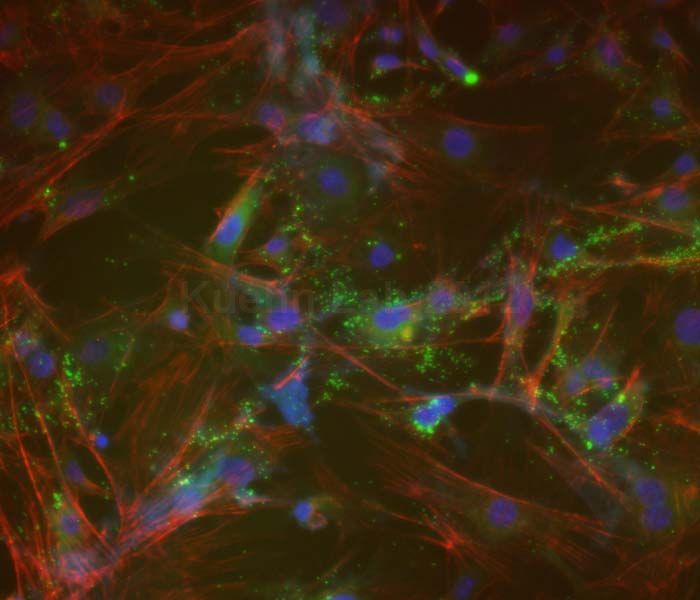
The source of these cells is, of course, crucial. In order to avoid immune rejection reactions to the transplanted tissue, it is desirable to use cells harvested from the patient. A patient’s native TM cells are difficult to obtain and may additionally be functionally compromised due to the effects of age-related stresses. In collaboration other laboratories at the University of Iowa Institute we are investigating if TM-like cells generated from induced pluripotent stem cell (iPSC-TM) can be used for this purpose. These cells can be created from the patient’s own dermal fibroblasts which are easily obtained through a skin biopsy. A second approach may be the use of mesenchymal stem cells that can be harvested from the patient's adipose tissue.
So far our results have been very promising. We have transplanted iPSC-TM into transgenic mice expressing a gene known to cause trabecular meshwork dysfunction, elevated IOP, and glaucoma in humans. Following transplantation the IOP decreased in recipient mice leading to enhanced survival of retinal ganglion cells, which is a very good indicator that the transplantation preserved vision.
This approach, which eliminates many of the ethical and practical concerns associated with the use of stem cells, offers the only clinically feasible solution to this challenge. Successful trabecular meshwork restoration would permanently restore IOP control and thereby reduce costs related to the life-long management of this chronic disease.
Last Updated: 11/10/2023